LCRF Scientific Advisory Board member Dr. Roy Herbst discussed new research in lung cancer recently on Bloom, Tampa Bay WFLA’s daily 1-hour show focusing on health and lifestyle. Watch below.
News

COVID-19 presents special challenges for physicians who treat lung cancer patients. Julie Brahmer, MD, spoke with Healio recently about what physicians need to know about lung cancer care during the pandemic.
Dr. Brahmer is a member of LCRF’s Scientific Advisory Board and Professor of Oncology at Johns Hopkins University School of Medicine.
Despite the current public health crisis, Dr. Brahmer sees hope for the future.
“Over the past couple of months, we’ve had even more options for treatment for lung cancer approved by the FDA and that continues to give us great hope for improving survival and improving their quality of life when diagnosed with lung cancer,” she said.
Watch this week’s update from LCRF Executive Director Dennis Chillemi.
We are #TogetherSeparately™
- View the recording of Free to Breathe Yoga and see highlights about the event.
- Read our recap of this week’s AACR virtual Annual Meeting.
- Get our latest information on lung cancer and coronavirus at LCRF.org/COVID19.
- Keep the dialog going in the Lung Cancer Community Facebook group.
Related: Read highlights from the ASCO Annual Scientific Meeting
The American Association for Cancer Research (AACR) held its second virtual Annual Meeting on June 22-24, 2020. The AACR Virtual Annual Meeting II meeting covered many of the latest developments from cancer research around the world. The focus of the program ranged from biology to drug development to policy and career development for scientists. Special sessions were also held to address current events such as the COVID-19 global pandemic and racism and racial inequities in cancer research.
Lung Cancer Research Foundation (LCRF) Scientific Advisory Board members and LCRF grantees were well-represented at this important scientific meeting.
LCRF grantee and newest member of the Scientific Advisory Board, Dr. Trudy Oliver from University of Utah Huntsman Cancer Institute presented on “modeling lung cancer subtypes in the mouse.” Dr. Oliver’s presentation emphasized the importance of understanding the organ affected by cancer—its genetic and biological make-up and how it functions. Down to the cellular level, we can understand how organs thrive and are affected by genetic mutations. Dr. Oliver spoke about several mutations that have been identified for SCLC and how they can be studied using mouse models that mimic the biology of cancer in humans. Ultimately, these mouse models help us find treatments based on what we learn from these mutations and how they operate.
LCRF grantee Dr. Lecia V. Sequist from Massachusetts General Hospital presented on “Low-dose CT scans for lung cancer screening in 2020: Areas of consensus and controversy and how to move forward.” Dr. Sequist presented on a critically important issue. Currently, there are only four types of available cancer screenings considered effective, one of them being for lung cancer. However, less than 5% of eligible adults in the U.S. actually get screened for lung cancer. This means lower rates of early lung cancer detection and poorer health outcomes. The 5-year survival rate for early stage NSCLC is almost 10 times higher than it is for late stage NSCLC. There is hope with the utilization of better technology and approaches to getting lung cancer screening widely available to the public.

LCRF Board Member and SAB Chair Dr. Katerina Politi from Yale Cancer Center, presented on “Incorporating translational research into clinical trials of targeted agents.” Dr. Politi’s presentation focused on how research findings in the lab influence the development of practical targeted therapy treatments. For example, the identification of biomarkers in tumors led to the eventual development of therapies to treat tumors harboring those specific mutations. Now, targeted therapies (targeting genetic mutations like EGFR, ALK, ROS1, etc.) are rapidly becoming a part of the standard-of-care for cancer patients. Clinical trials will continue the critical work around the development and application of these therapies.

LCRF SAB member Dr. Roy S. Herbst from Yale University School of Medicine, presented on “Combination strategies with IO agents.” Much like the rapid deployment of targeted therapies to treat cancer patients is the expanded use of immunotherapy treatments. Immunotherapy is now widely used across all lung cancer diagnoses and often in combination with other therapies such as chemotherapy. However, it is important to continue to test for safety and efficacy as immunotherapy does not always benefit each lung cancer patient equally. Clinical trials are being conducted to better understand both the safety and duration of benefit of immunotherapy with other treatments for cancer patients.
A member of former LCRF grantee Dr. Jessie Yanxiang Guo’s laboratory, Vrushank Bhatt from Rutgers Cancer Institute of New Jersey, presented their research titled “Autophagy inhibition sensitizes Liver Kinase B1 (LKB1) – deficient Kras-driven lung tumors to MEK inhibitor Trametinib.” The presentation highlighted two commonly occurring mutations, LKB1 and KRAS, which occur in NSCLC. When co-mutated, these alterations tend to drive the development of aggressive forms of lung cancer, making it harder to treat. Dr. Guo and her team’s research explored how tumor cells with these mutations might be better targeted with a drug called trametinib by interfering with a metabolic process called autophagy. Through this understanding, their work aims to demonstrate an additional use for this particular targeted therapy.
Special topics were also part of the AACR Virtual Annual Meeting II’s program. This year’s global COVID-19 pandemic has taken a toll on the way we conduct cancer research and how we understand cancer treatment and survivorship. A special session on COVID-19 and Cancer Research explored the importance of building immunity and understanding how the human body responds to this novel virus. The more we begin to understand COVID-19, the better we can protect the cancer community. Another special session on Racism and Racial Inequities in Cancer Research explored the various factors that inhibit minority representation and/or participation in clinical trials, both on the patient side as well as the researcher side. The discussion identified ways to combat this disparity and continue the momentum of racial equity in cancer research going forward.
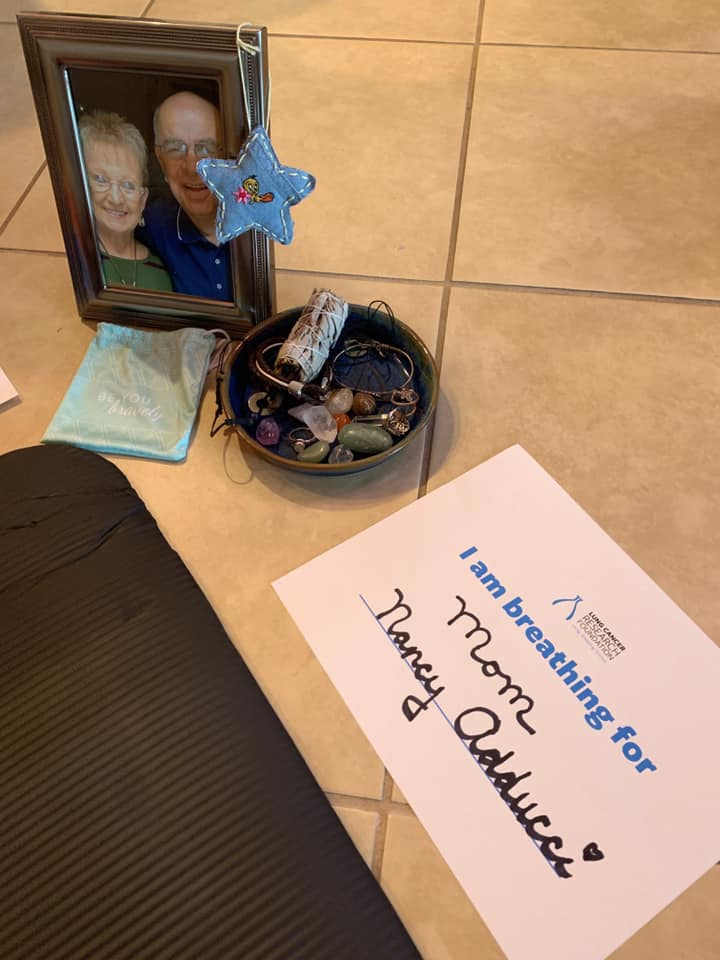
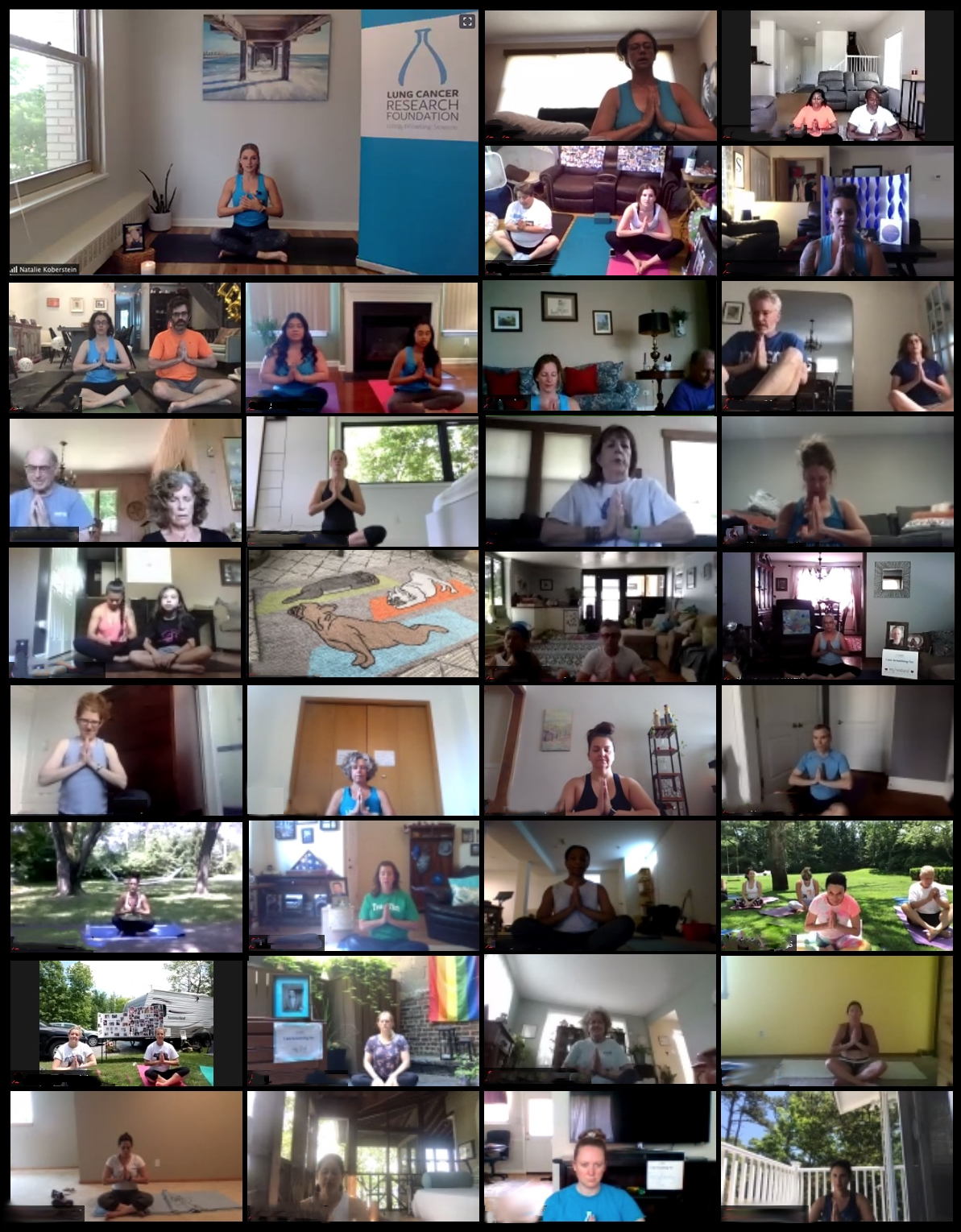
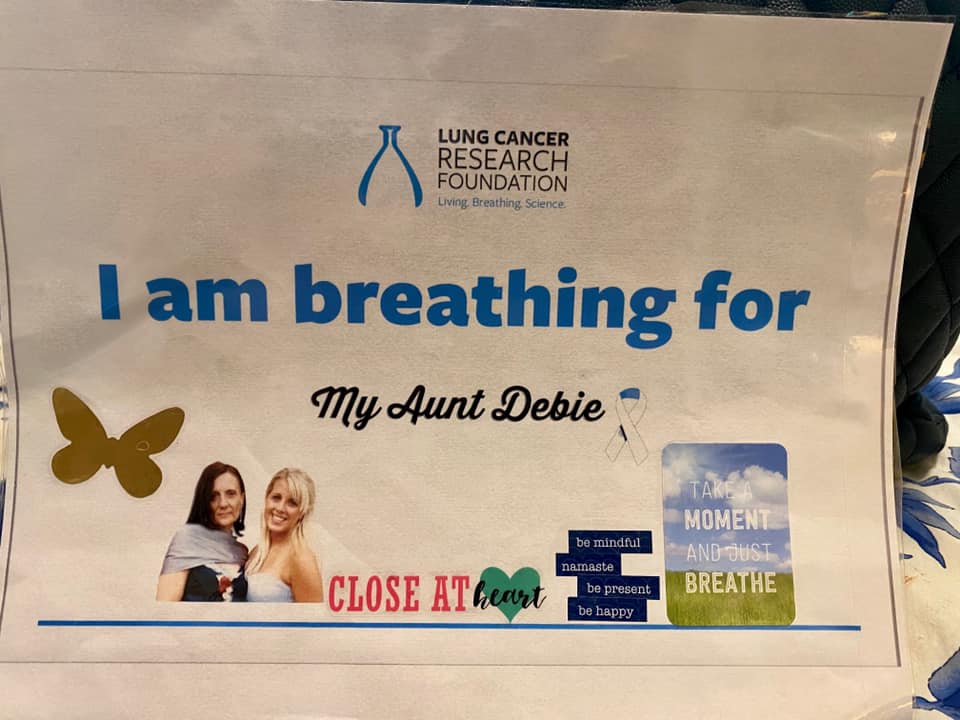
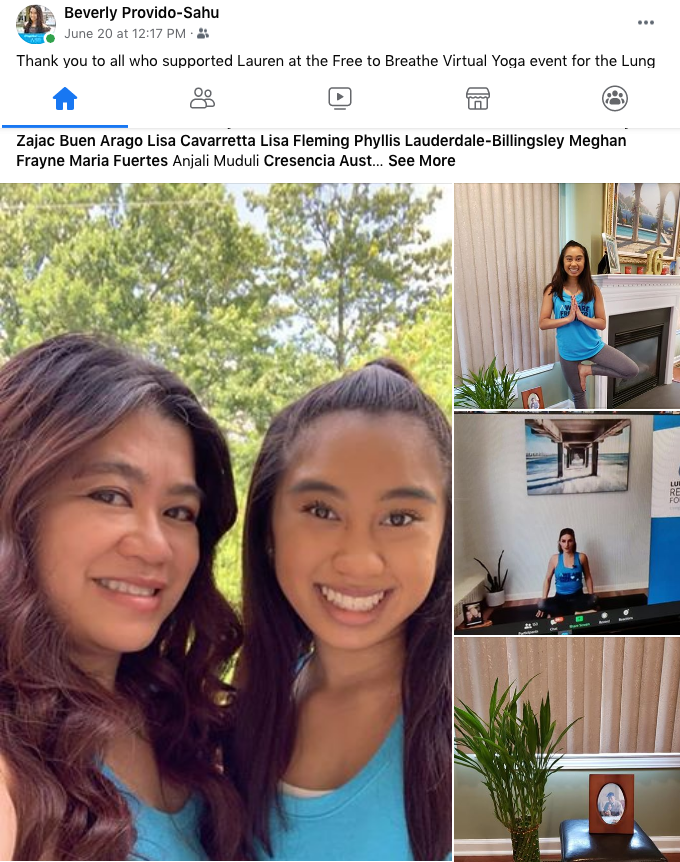
Hundreds of participants tuned in for LCRF’s first-ever virtual yoga event on Saturday, June 20, 2020. More than 900 people representing 43 states registered for the livestream, including 200 people who have received a lung cancer diagnosis – a record turnout of survivors for a single event.
As of event weekend, supporters have raised $54,000! You can still donate and support lung cancer research!
Watch the entire event below!
LCRF Executive Director Dennis Chillemi welcomed everyone and introduced Dr. Khinh Ranh Voong, Assistant Professor of Radiation Oncology and Molecular Radiation Sciences for Johns Hopkins Medicine. Dr. Voong, a previous recipient of an LCRF research grant, shared her insights about how research is shaping the future. (Dr. Voong’s introduction is at 26:40.)
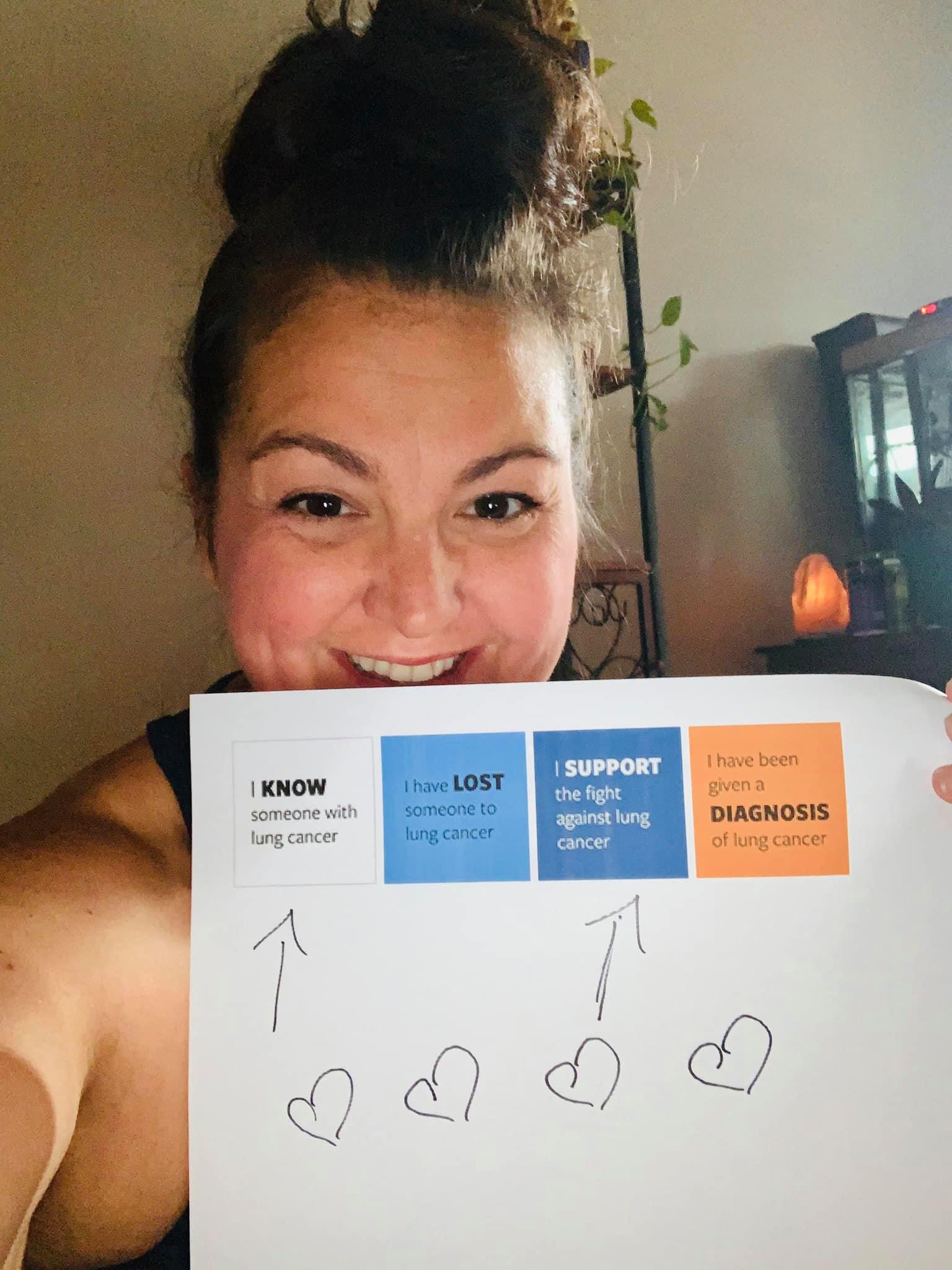
Jaymie Bowles, joining from Georgia, told about her journey after being diagnosed with Stage IV lung cancer two years ago. (Jaymie is introduced at 31:19.) She pointed out that she was wearing the color orange to represent “I have been given a diagnosis of lung cancer.”
Several others explained how the color they were wearing represented their connection to lung cancer. White means “I know someone with lung cancer.” The color turquoise means “I have lost someone to lung cancer.” Navy blue means “I support the fight against lung cancer.”
From her home near Chicago, yoga instructor Natalie Koberstein led meditation followed by a gentle yoga flow. (Yoga begins at 39:43.) Natalie lost her father to lung cancer five years ago and has been involved with Free to Breathe Yoga since its beginning.
Take a look at highlights from social media below! (Click to view full sized)
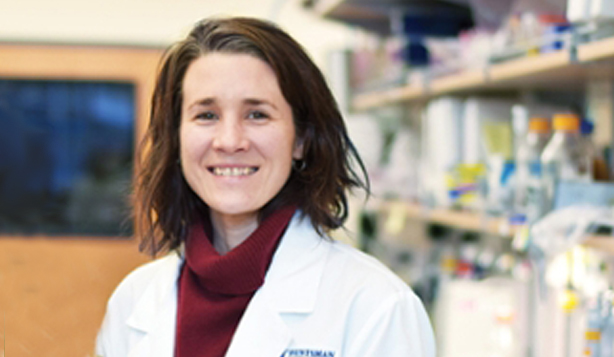
NEW YORK, NY (June 22, 2020) — The Lung Cancer Research Foundation (LCRF) today announced that Trudy Oliver, PhD, has joined its Scientific Advisory Board. Dr. Oliver is an Associate Professor of Oncological Sciences at the University of Utah’s Huntsman Cancer Institute (HCI), where she has served since 2011, and is an HCI Endowed Chair in Cancer Research. Serving on a number of administrative committees, Dr. Oliver has also actively participated in several strategic initiatives at HCI.
Dr. Oliver obtained her PhD in pharmacology and cancer biology from Duke University, working in Rob Wechsler-Reya’s laboratory. Following graduate school, she joined Terry Van Dyke’s laboratory at the University of North Carolina – Chapel Hill, and then completed her postdoctoral fellowship in Tyler Jack’s laboratory at the Koch Institute for Integrative Cancer Research at MIT before joining the University of Utah and Huntsman Cancer Institute in 2011. Her research is devoted to understanding mechanisms of cancer biology with a focus on lung cancer; she has developed novel mouse models of squamous and small cell lung cancer using experimental approaches including an integration of mouse genetics, molecular and cellular biology, biochemistry, genomics, preclinical therapeutics and in vivo imaging.
Dr. Oliver is a 2018 recipient of LCRF’s Wiliam C. Rippe Award for Distinguished Research in Lung Cancer, which supported, in part, her laboratory’s continuing study of the MYC genetic alteration that drives how small-cell lung cancer (SCLC) tumors develop. Her research discovered that SCLC tumors caused by the MYC protein are more aggressive, spread faster and respond differently to therapy. Her team discovered that ADI-PEG20, an enzyme that breaks down the amino acid arginine, is highly effective in MYC-positive genetically-engineered mouse models and human patient-derived tumors, resulting in a promising breakthrough. She is also personally affected by lung cancer; her mother’s low-dose CT scan showed a nodule that they chose to monitor – which helps to fuel her passion for changing outcomes for patients living with lung cancer.
“I am excited to welcome Dr. Oliver to LCRF’s Scientific Advisory Board and look forward to working with her to continue the Foundation’s commitment to funding outstanding lung cancer research and investigators,” said Dr. Katerina Politi, Chair of LCRF’s Scientific Advisory Board. “Her commitment to improving outcomes for lung cancer patients is reflected in her work, and we’re thrilled she has joined us.”
Dennis Chillemi, Executive Director of LCRF adds, “Dr. Oliver’s expertise in lung cancer biology has already made a significant impact on the lung cancer community, and we look forward to her valuable input as a member of the Scientific Advisory Board.”
LCRF’s Scientific Advisory Board includes renowned scientists, physicians and thought leaders spanning a broad range of disciplines in lung cancer research who leverage their collective experience and expertise to maintain the objectivity of the grant selection process and help to ensure that LCRF continues to fund research of the highest caliber. The group is responsible for the review of grant applications and providing opinions and strategic input to LCRF’s Board of Directors on relevant topics. Members are selected and recruited based on their level of expertise, prominence in the field of lung cancer research, and commitment to LCRF’s mission.
# # #
About the Lung Cancer Research Foundation®
The Lung Cancer Research Foundation® (LCRF®) is the leading nonprofit organization focused on funding innovative, high-reward research with the potential to extend survival and improve quality of life for people with lung cancer. LCRF’s mission is to improve lung cancer outcomes by funding research for the prevention, diagnosis, treatment and cure of lung cancer.
To date, LCRF has provided $34 million in research grants to investigators around the world. In addition to funding lung cancer research, the organization focuses on lung cancer awareness and educational programs. The Foundation also hosts community events nationwide through its Free to Breathe® Events Program.
Watch this week’s update from LCRF Executive Director Dennis Chillemi.
Join us #TogetherSeparately™
- Register for virtual Free to Breathe Yoga, taking place TOMORROW, June 20!
- Get our latest information on lung cancer and coronavirus at LCRF.org/COVID19.
- Keep the dialog going in the Lung Cancer Community Facebook group.
The American Cancer Society has recently updated their guidelines on diet and physical activity for cancer prevention. The guidelines serve as evidence-based recommendations individuals can take to reduce their risk of cancer. The key recommendations include:
- Maintaining a healthy weight throughout the lifespan
- Engage in physical activity as follows:
- 150-300 minutes or more per week of moderate intensity -OR-
- 75-150 minutes or more per week of high intensity
- For children/adolescents: 60 minutes or more per day of moderate or high intensity
- Keeping a healthy diet that limits or does not include:
- Red and/or processed meats
- Beverages with added sugar
- Highly-processed foods and refined grain products
- Avoiding alcohol or limiting alcohol consumption as follows:
- For women: No more than 1 drink per day
- For men: No more than 2 drinks per day
The guidelines also included actions the broader community can take such as increasing the accessibility of fresh and affordable foods, spaces for community exercise and leisure physical activity, and much more. Finally, the guidelines conclude with answers to common questions about cancer and cancer prevention such as the role of supplements, special diets and food preparation.
More information can be found here.
LCRF’s #Together Lung Cancer Community Talk on Thursday, June 11 focused on recent FDA approvals and what they mean for lung cancer patients. Our guest was Alexander Drilon, MD, a medical oncologist who treats lung cancer patients at Memorial Sloan-Kettering Cancer Center. Dr. Drilon is a 2012 LCRF grant recipient and a leading expert in clinical research in his position as Research Director, Early Drug Development.
After the talk, Risë Van Doosselaere offered an optional yoga flow for the group. (This section begins at 00:59:39 in the video.)
#TogetherSeparately livestreams provide an opportunity for the lung cancer community to connect face-to-face and discuss current issues and challenges. Watch the full livestream below. You can also download a PDF chat transcript.
Watch this week’s update from LCRF Executive Director Dennis Chillemi.
Join us #TogetherSeparately™
- Register for virtual Free to Breathe Yoga, taking place Saturday, June 20.
- Get our latest information on lung cancer and coronavirus at LCRF.org/COVID19.
- Keep the dialog going in the Lung Cancer Community Facebook group.